Choosing the Best BI for Your Facility
Are BIs the Validation Tool for You?
Biological indicators (BIs) containing Geobacillus stearothermophilus have become a standard and reliable source in the world of high-level disinfection and sterilization. These tools provide valuable information about the level of microbial resistance to a sterilization treatment. While biological indicators can be employed in any facility, they are most commonly implemented in healthcare facilities, the pharmaceutical industry, and laboratories to validate the sterility of a process. For example, in healthcare, they would be employed to help ensure sterilization of medical devices. For life science, they would be included to ensure a laboratory was sterile after a biodecontamination cycle or to ensure contamination control of sensitive areas, like pharma production sites. They have become popular in these environments because these facilities have a higher risk of developing microbial contamination or require regular strict environmental monitoring to ensure compliance.
Where are biological indicators used?
- Pharmaceutical Manufacturing: Many pharma facilities are required to maintain sterile environments free of contaminants in accordance with GMP (Good Manufacturing Practices) guidelines. The pharmaceutical industry often employs BIs in drug manufacturing facilities to ensure validation of contamination control methods following a sterilization treatment. In these cases, BIs would be used to determine Sterility Assurance Levels (SAL).
- Healthcare: Healthcare facilities utilize BIs to determine if the autoclaving of surgical and other medical equipment has been successful in its sterilization process. Sterilization chambers for heat sensitive equipment are also commonly implemented and BIs can be used during this process to validate sterility. (Since ethylene oxide is a common sterilant in this industry, Bacillus atrophaeus BIs are frequently used.) Geobacillus stearothermophilus are used most frequently in hospitals as they can be paired with steam sterilization, vapor hydrogen peroxide, and hybrid hydrogen peroxide treatments.
- Laboratories: Labs often deal with cross-contamination concerns that may lead to the loss of valuable and expensive research. Because of this, BIs are utilized often to ensure adequate sterilization or disinfection treatments have been performed.
Benefits of Biological Indicators
Biological indicators are a resource that can be implemented for many high-level disinfection or sterilization treatments. They can be employed with a variety of chemicals like ethylene oxide, vapor hydrogen peroxide, hybrid hydrogen peroxide, dry heat, steam (autoclave), chlorine dioxide, and formaldehyde. BIs are generally paired with chemicals to which they are most resistant. This allows the treatment to be challenged and validated. For example, Geobacillus stearothermophilus is resistant to steam and vapor hydrogen peroxide (VHP) so these processes are paired with these biological indicators during a treatment. Ethylene Oxide (EtO) and Dry Heat are generally paired with biological indicators containing Bacillus atrophaeus spores, as those spores have been shown to be most resistant to those processes during testing. 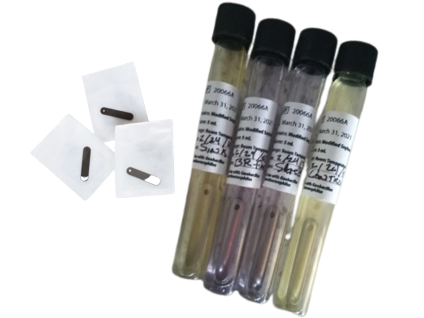
How do biological indicators work, and which BI is best for you?
Biological indicators are comprised of a specific carrier material, a resistant bacterial spore strain, and a primary packaging material. This combination of spores and materials is responsible for the resistance of that BI in decontamination or sterilization processes. Common carrier materials are cellulose/paper, stainless steel, and even quartz. Carrier materials are chosen in the initial development stage, taking into consideration their compatibility with the specific processes and industry needs. Common primary packaging materials are glassine and Tyvek. Whereas glassine is the legacy material chosen for most penetrative processes, Tyvek is commonly used in processes using hydrogen peroxide.
For most applications, the inoculated carrier should remain inside the primary packaging during exposure. The biological indicator manufacturer assesses the resistance of the inoculated carrier material when maintained in this packaging. Removing the carrier materials from the primary packing prior to exposure is not recommended.
Biological Indicator Carriers: Types and Uses
- Paper Carriers- strips or discs: Paper is the chosen carrier material for processes like steam and gaseous sterilants which can easily penetrate through the paper.
- Stainless Steel Carriers- discs or coupons: Stainless steel carriers are often used because they mimic the surfaces commonly decontaminated in laboratory spaces. Paper carriers may not be compatible for biological indicators used in high temperature dry heat processes above 200˚C and stainless steel may be more appropriate for higher temperature applications.


- Tyvek Enclosed: Metal coupons that are enclosed in Tyvek/Tyvek pouches are used to add a layer of protection, but also serve to challenge the testing even further due to the Tyvek membrane as a barrier instead of an exposed bare coupon. These are typically used with vapor hydrogen peroxide and hybrid hydrogen peroxide and are the federally recommended method.
- Self-Contained BIs: Self-contained biological indicators are preferred for a variety of applications. The term self-contained is used for these products because there is not a need for post-process removal of the inoculated carrier material and subsequent culturing in media. The media is contained within the BI and is only allowed to come into contact with the inoculated biological portion until after the cycle is completed. Biological indicator users prefer these types of BIs, as they are easier to use and lower the risk of post-process contamination.
- Ampoule BIs: Ampoule type biological indicators were developed specifically for monitoring the sterilization of liquids. The ampoule contains the spores suspended directly in the growth media with a pH indicator. The ampoules are suspended at the slowest to heat a portion of the container of liquid which may be a reagent or media utilized in a laboratory, IV solution, or pharmaceutical component. Once the sterilization cycle is complete, the ampoule is removed from the liquid and placed directly into incubation. An ampoule which remains the original color throughout incubation is indicative of a passing sterilization cycle and a color change in the media indicates insufficient sterilization of the liquid.
For most purposes, bacterial spores are utilized for their high resistance to heat and chemicals. BIs also work off the assumption that, if you can kill high-level bacterial spores (population of 100,000,000 or more), you can also effectively kill organisms beneath them on Spaulding’s hierarchy like bacteria, viruses, and fungi.
Biological Indicator Placement, Collection, and Incubation
After choosing a BI for your facility, it is now time to place it for a treatment cycle. When it is time for the decontamination to commence, the carriers are placed in the space receiving a high-level disinfection or sterilization and in areas expected to be most challenging. Immediately after the treatment cycle is completed, the BIs are carefully removed and are aseptically cultured in broth.
Common Types of BI Culture Broth
Common types of broths include trypticase soy broth (TSB), Soybean Casein Digest Medium (SCDM), or proprietary media formulations with pH indicators which are provided by the BI manufacturer.
Incubating and Analyzing Biological Indicators Results
The BIs are subsequently incubated at the specified temperature for 7 days or at the appropriate number of days recommended by the BI manufacturer when a reduced incubation time (RIT) has been determined. If, after incubation, turbidity or a color change has occurred in the media, the spores were not killed during the treatment cycle. If the media remains clear or the color has not changed, the spores were killed during the treatment cycle, and the treatment was successful. Generally, if using numerous biological indicators with a 10^6 log initial spore population to challenge the cycle, the total kill of the BIs aligns with 8 spore log reductions being achieved. In the case of aseptic environments, multiple BIs or even triplicate BIs may be used in a treatment cycle when targeting a specific Sterility Assurance Level (SAL) is desired.
Downsides to BIs
While BIs are a valuable resource in multiple industries, there are a few downsides to consider before you use them in your facility. BI results are not immediate and can take up to 7 days to validate a sterilization treatment. Human error is a common concern because not using proper aseptic techniques while handling the BIs can contaminate the sample and skew your results. Using BIs past their expiration date or failing to store BIs per manufacturer recommendations can lead to inaccuracies in the outcomes. In rare cases, errors can occur when a lab is manufacturing the BIs that may result in false-positive results. For these reasons, some facilities will choose to also incorporate the use of enzyme indicators.
Summary
Understanding biological indicators and their variations will help facilities achieve the maximum from their sterilization methods, especially when considering the addition of any gaseous systems like vapor hydrogen peroxide (VHP) and hybrid hydrogen peroxide (HHP). These indicators are widely accepted by multiple Federal agencies; therefore, the use of these for validation purposes will likely extend long into the future. CURIS System utilizes Biological Indicators of Geobacillus stearothermophilus and Bacillus atrophaeus in Tyvek/Tyvek pouches and with populations of ≥6 logs to ensure that treatment cycles are efficacious and treated areas remain safe.
To learn more about how CURIS System can be an efficacious disinfection tool for your facility that can be validated with biological indicators, visit our website at curissystem.com.
References
Office of Device Evaluation, & Murphy, S., Biological Indicator (BI) Premarket Notification [510(k)] Submissions1–20 (2007). Rockville, Maryland; Center for Devices and Radiologic Health.
Albert, H., Davies, D. J. G., Woodson, L. P., & Soper, C. J. (1998). Biological indicators for steam sterilization: characterization of a rapid biological indicator utilizing Bacillus stearothermophilus spore-associated alpha-glucosidase. Journal of Applied Mircobiology, (85), 865–874.
Aaadmin, Author: aaadmin, & Author: (2017, March 7). What is a biological indicator?: Biological indicators. Mesa Labs Biological Indicators. Retrieved March 17, 2022, from https://biologicalindicators.mesalabs.com/2016/10/14/what-is-a-biological-indicator/
Centers for Disease Control and Prevention. (2018, March 22). Sterilization: Monitoring. Centers for Disease Control and Prevention. Retrieved March 17, 2022, from https://www.cdc.gov/oralhealth/infectioncontrol/faqs/monitoring.html
Protak Scientific http://protakscientific.com, & Author: (2017, February 3). What are biological indicators? Protak Scientific. Retrieved March 31, 2022, from https://www.protakscientific.com/what-are-biological-indicators/